Identifying and Treating Pelvic Organ Prolapse
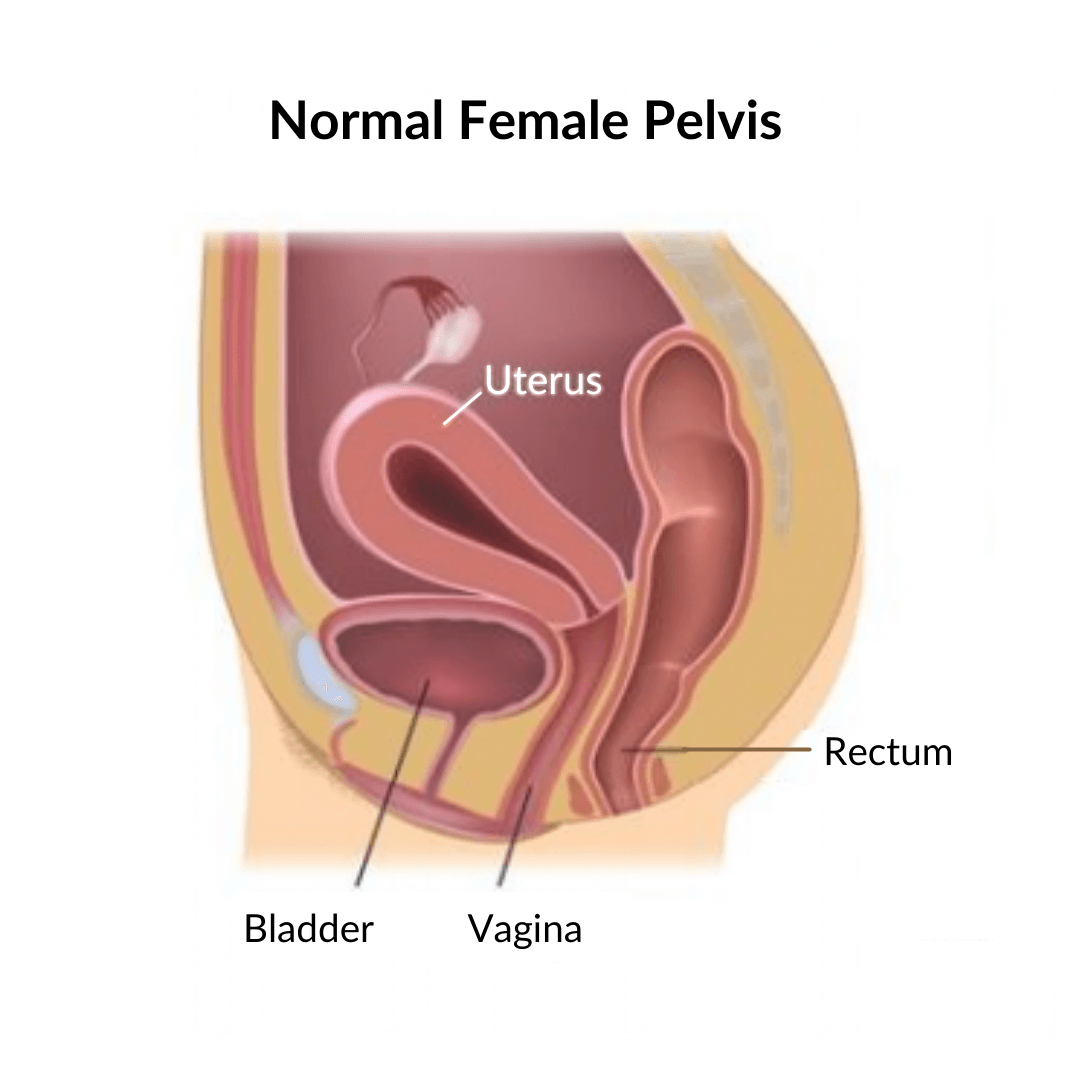
Pelvic organ prolapse, also known as POP, is a disorder of the pelvic floor. It is created by damage or weakening of the muscles in the pelvis through trauma such as pregnancy and childbirth, lifting heavy weights, chronic constipation or even a long-term cough that causes straining.
You may not know it, but prolapse can happen to women or to men.
In women, when the pelvic floor is unable to support the organs, one or more of them can slip and descend into the vagina. This is known as a prolapse.
This is the second part of our two-part feature on POP. You can find a full definition and what you can do to protect yourself from being affected by it in our previous post on what prolapse is and how to avoid it.
Can You Prevent Pelvic Organ Prolapse?
As it happens when the muscles of the pelvis are weakened, the best way to prevent POP happening to you is to maintain good pelvic health. There are a number of steps you can take to help avoid or lessen the symptoms; for example, lifting properly, keeping good posture, a healthy weight and dealing with constipation. And if you have a smoker's cough, then it will also be good to ditch the cigarettes.
The best way to ensure your pelvic floor is able to function well is through special exercises.
You might know these exercises as Kegel exercises or Kegels, after the American gynaecologist who first promoted them as a way for women to keep their pelvic floor strong and functional.
However, there are a number of conditions or events that may have an adverse effect on these muscles and cause prolapse regardless of how well you manage your pelvic floor exercises.
Types of Pelvic Organ Prolapse
Prolapse can happen to any of the pelvic organs. A woman suffering from this condition can have the bladder, uterus, vagina or rectum bulging out of the vagina.
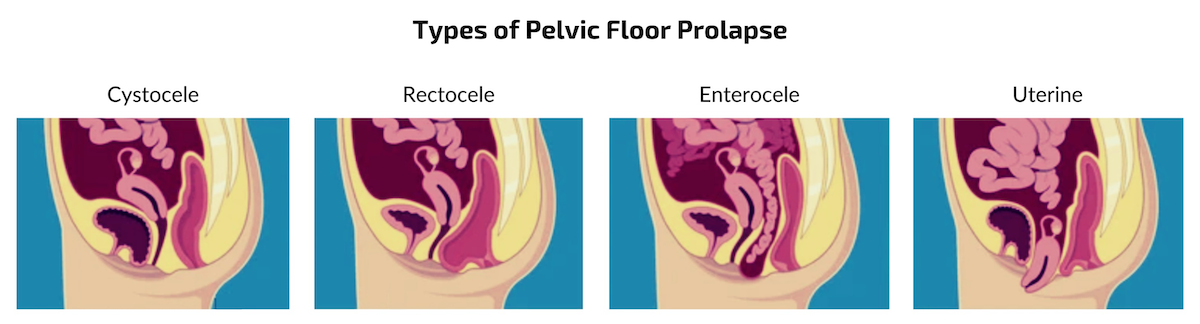
The different types of prolapse are:
- Cystocele - Also called anterior prolapse, this is when the bladder slips into the vagina.
- Urethrocele - Prolapse of the urethra (the tube that carries urine).
- Uterine prolapse - When the uterus descends into the vagina.
- Vaginal vault prolapse - Prolapse of the vagina, when the top of the vagina sags down after hysterectomy.
Posterior wall prolapse - This occurs when part of the bowel pushes into the wall of the vagina. When it concerns the small bowel bulges forward into the upper wall of the vagina, it is called enterocele. When the end of the large intestine pushes against the back of the vaginal wall, it is called rectocele.
Stages of Pelvic Organ Prolapse
There is a grading system called the Pelvic Organ Prolapse Quantification System (POP-Q) which describes the severity of POP. There are four stages; the first stage may be a minor movement of the organ, increasing incrementally to stage four which involves the organ protruding out of your body.
The stages of pelvic organ prolapse are:
Stage 1 - mild
At this stage you might show no symptoms. The organs are still adequately supported by the muscles of the pelvis.
Stage 2 - moderate
People with moderate pelvic organ prolapse might be experiencing some symptoms such as a dragging, heavy or full feeling in the pelvis. There might also be some pain or discomfort during sex as well as back pain. The organ has dropped from its natural position but is still inside the body.
Stage 3 - severe
With a prolapse that has reached this stage, there will be a number of frequent and disturbing symptoms like feeling of not emptying properly bladder or bowel. There may be a bulge or lump in the vagina. A sudden stress such as sneezing, coughing or laughing can cause the organ to protrude outside the vagina.
Stage 4 - complete
When you have complete prolapse, you will probably experience all of the symptoms described above. You will be in extreme discomfort and will have a bulge outside your vagina.
These symptoms sound frightening, and they can certainly cause discomfort, embarrassment and pain. But the good news is that prolapse isn't life-threatening. Part I of our blog on POP gives you the steps you can take to avoid being affected by this condition.
If you find you are already experiencing these symptoms and you fear you might be suffering from prolapse, seek advice from a women's health physiotherapist. They will be able to diagnose your condition accurately, give you treatment and some reassurance too.
Treatment for Pelvic Organ Prolapse
There are several ways you can treat and manage this condition, including exercise, products to help support your muscles and organs and, in the worse case, even surgery.
Pelvic Floor Exercises
A pelvic floor physiotherapist will typically recommend specific, targeted pelvic floor exercises. Kegel exercises alone are unlikely to completely reverse a prolapse, but they will certainly improve your condition, and your symptoms may be significantly improved through this activity.
Biofeedback
It might be difficult to identify or isolate the right muscles for your Kegel exercises to be effective. In that case, biofeedback can help. Using special instruments either inside or outside the vagina, a biofeedback therapist can measure the activity of your muscles. That will teach how to stop using the wrong ones and start using the right ones.
Pelvic Floor Stimulation
Stimulation of the muscles of the pelvis can be achieved using small amounts of electrical current, making the muscles tighten or contract, which in turn strengthens them. This treatment can be applied within a clinical setting or by using a home system. While this stimulation can be very beneficial in helping to "wake up" the muscles, it should not be used as a replacement for a proper strengthening programme.
Pessaries
In situations where exercises cannot completely resolve POP, a silicone pessary is a non-surgical treatment option. The pessary is specially made to fit you and, when inserted into the vagina, provides comfort from your symptoms through structural support. Pessaries need to be removed and cleaned regularly.

Surgical Treatment
In extreme cases, reconstructive surgery for POP is a treatment option to correct the problem and improve bowel, bladder and vaginal function. There are a number of different techniques that can be used in this surgery, for example laparoscopy, through the vagina or through an incision in the abdomen. It's important to note, however, that 30% of prolapses recur after surgery.
The different types of surgical repairs are:
- Repair of Cystocele or Rectocele - repair to a prolapsed bladder, urethra or rectum and small bowel.
- Vaginal Vault Suspension - repair of the vaginal wall, commonly performed laparoscopically.
- Hysterectomy - complete removal of the uterus.
- Vaginal Obliteration - most of the entire vaginal lining is removed, and the vagina is sewn shut. Sexual intercourse is no longer possible after this procedure, and it is not reversible.
With surgical options come greater risk, and they are not always 100% effective.
If you're suffering from this condition, a pelvic physiotherapist can help you. If your symptoms have occurred as a result of pregnancy, then you would benefit from a Mummy MOT. That will give you a full post-natal checkup to examine not only your pelvic floor, but every part of you that has been affected by pregnancy, labour and the postpartum period.
For more information about physiotherapy treatments for pelvic organ prolapse or other women's health issues, call Magdalena on 07877 017 936 or drop PelviCare an email. Alternatively, you can book an appointment online.
PelviCare Women's Health Physiotherapy is located in Greenwich, London, serving women across South London, East London, Essex, Kent and beyond.
Recommended Articles:
Pelvic Organ Prolapse - What It Is and How to Avoid It
How Women's Health Physiotherapy Can Help with Urinary Incontinence